Although SIRT is most commonly used as a palliative treatment in patients with inoperable malignancy in the liver, it can also be performed in some instances to downstage patients to subsequently have surgery and to avoid disease progression in patients waiting for resection. Colorectal metastases treated with SIRT are usually resected 3-9 months after treatment. It is important that the operating surgeon knows about the embolisations previously performed during the Liver Angiogram before the SIRT and the parts of the liver that were treated with SIRT. Well planned surgery after SIRT is safe.
In patients with unilateral, primary and secondary liver tumours, the ability to perform potentially curative surgery can be hampered by insufficient liver volume in the future liver remnant (FLR) that will be left following surgery. In particular, patients who have cirrhosis or chemotherapy-associated liver injury often require >30% FLR. Since popularised by Makuuchi in 1990, portal vein embolization (PVE) of the tumour-bearing liver has become the technique of choice in most Liver Centres to induce contralateral liver hypertrophy. Unfortunately, this leaves the ipsilateral tumour(s) untreated, often allowing disease to progress. Lobar selective internal radiation therapy (SIRT) not only treats the tumour in the embolised lobe, but can often result in a volume reduction of the ipsilateral tumour-bearing lobe and hypertrophy of the contralateral lobe, thus increasing the chances of a successful liver resection. In recent studies, SIRT was most effective in minimizing the risk of tumour progression in the treated lobe and had more of an effect on total liver volume, making it a more suitable modality for selected patients with substantial unilateral disease burden. Many Liver Centres are now using SIRT in preference to PVE in selected patients as a valuable bridge to potentially safe liver resection in patients who are borderline resectable.
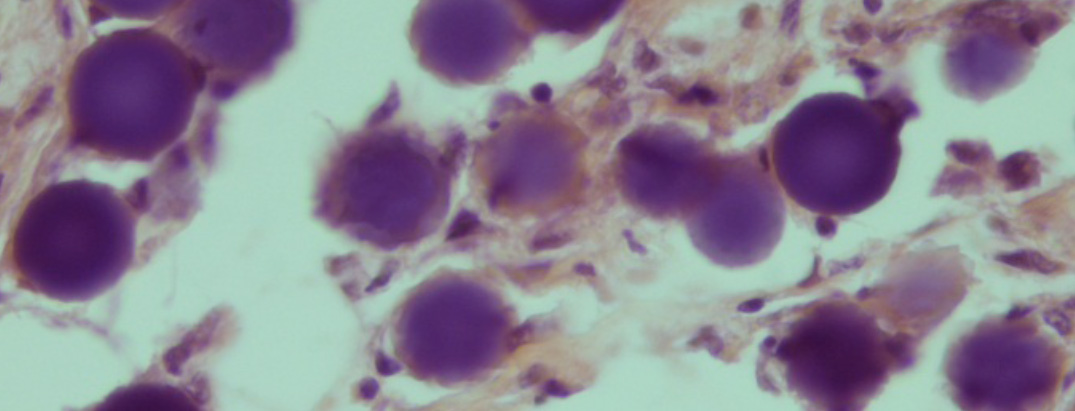
Specimens from liver surgery in patients previously treated with SIRT are cut up and reported using the guidelines developed for these specimens by the Royal College of Pathologists (http://www.rcpath.org/publications-media/publications/datasets/Liver.htm). In resected metastases, in general, a number of histological features have been suggested as having prognostic significance (reviewed in Histopathology 2013, 63, 149-156.) In SIRT cases, the microspheres are seen in blood vessels both in the surrounding liver and within the tumour. The tumour may show necrosis, mucinous change and fibrosis in varying combinations while inflammatory changes are relatively inconspicuous (J Clin Pathol 2013; 66:205-211) (Figures 1 and 2). The changes seen in the surrounding liver are usually mild are due to the presence of space occupying lesion.

There is a restricted access forum for all clinicians involved in the SIRT procedure to help share best practice and experiences. If you have or you would like to share your experiences or you want to find out more about the procedure and the latest clinical developments, please join our community.
Click here to join or sign-in

There is a designated site for SIRT patients, their families and carers called My SIRT Story.
Click here to find out more
